How to make your medical spa impossible to compete with.
/The world is changing rapidly — you might have heard to all of the A.I. tools like ChatGPT, Bard and the rest… and what used to work for cosmetic clinics and providers in the past is no longer enough to compete in today's market.
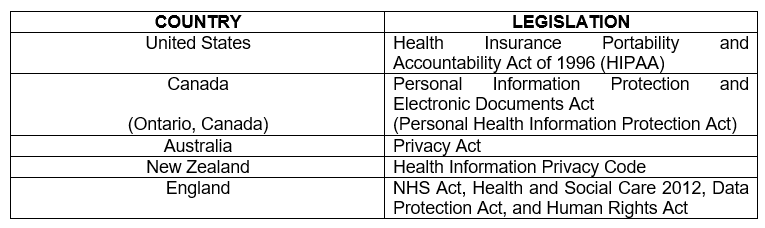
There’s been a 63x increase in telemedicine since 2020 (Yep. Covid.) [1]. Additionally, a whopping 71% of all in-person clinical visits can now be done remotely [1]. Patient expectations have shifted too. The result is that 81% of existing patients are open to switching providers at any time[1]. Patient churn, redundant and inefficient practices, and lost revenue opportunities are killing your growth, and your practice.
With increased competition, evolving patient expectations, and the need for a unique value proposition, it's crucial to find you unfair advantage and put it to work — you need to be impossible for others to compete with.
Just because you’re unaware of the losses doesn’t make them any less real. Remember this; you can’t just be good — you have to be better than everyone else. Patients have access to everyone and all the information they need, and they will move to whomever they feel best fits them.
Finding Your Unfair Advantage
In this new healthcare landscape, there will inevitably be winners and losers. To ensure that your clinic is among the winners, you need to find your unfair advantage and learn to compete in ways that other’s can’t simply copy, and they’re working hard too. Think of it as ‘asymmetrical competition’ — the ability to redefine the playing field and the rules of the game.
Hint: It’s not going to be your IPL or laser or the lemon water or any of the bullshit that you hear from the sales reps about how they’re going to put you on their vendor website.
But you have a real problem…. you’re not actually much different.
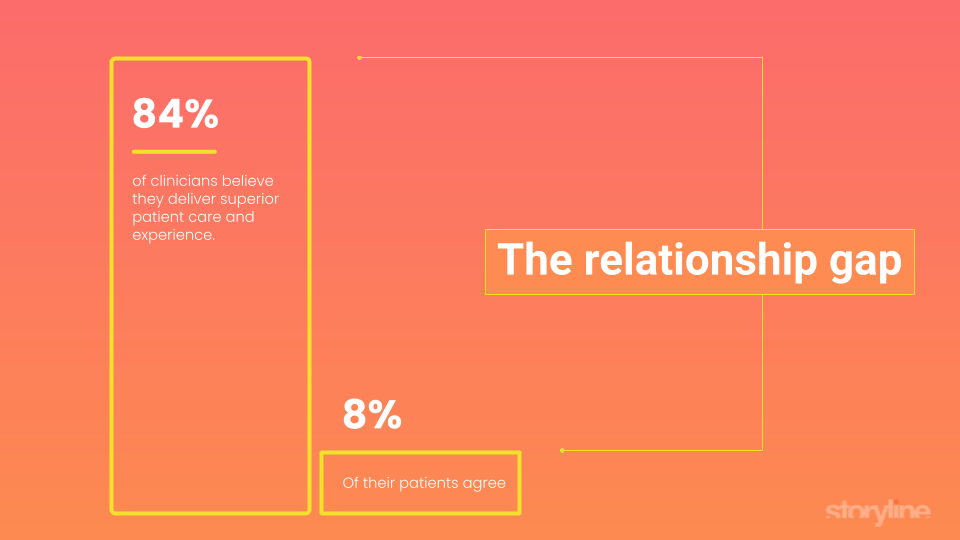
If you’re like most providers, you’re kidding yourself. A massive 84% of clinicians believe they deliver superior patient care and experience, but only 8% of their patients agree.
While it’s most likely that your current patient care and experiences are lockstep with what they can get down the street. Your staff is similar, your offerings are largely the same, and your pricing too. The fact that you’ve got a different RF device or were the first to perform ‘whatever-treatment-you-want-to-insert-here’ for longer than your competitors is irrelevant.
Guess what; nobody cares. That’s just more marketing b.s. and you should not delude yourself based on hopeful thinking.
What does a real competitive advantage look like?
Success in this new world isn’t easy. It requires a combination of factors; exceptional patient experiences, streamlined operations, and new business models. All of these are massive opportunities for those who are smart enough to adapt and use them — especially since most clinics will be too slow to make the needed changes.
There are new technologies that provide a clear path to market dominance.
Patient experience: Creating and automating exceptional and personalized patient experiences that go far beyond current tools to build strong patient relationships, and real loyalty.
Productivity: Automating redundant tasks, personalize patient experiences, and build strong relationships with their patients.
New business models: Creating new ‘hybrid’ business models that provide recurring revenue and subscriptions as well as your current services model.
There are technologies you can use do do all of these things.
Imagine your clinic where your staffs productivity is increased by 4x, and you’re increasing high-touch patient interactions by 260% (without any additional time)[3], and you’re generating recurring revenue from subscriptions (since we’re now in a subscription economy).
In this future, your clinic is more efficient, patient-focused, and ultimately, more successful.
You can’t just work harder, or do this by yourself.
Several obstacles stand in the way of achieving this vision of success for your clinic. In the past, you’ve just worked longer hours and hired more bodies, but those strategies have had diminishing returns for a while. It’s no longer a workable solutions, especially in competitive markets. This focus on manual work and care delivery forces multiple problems into your clinic:
Time-consuming, manual tasks that prevent healthcare providers from focusing on patient care.
Difficulty in personalizing patient experiences and building strong relationships.
Inefficient workflows and processes that hinder overall clinic productivity.
To overcome these obstacles, you need tools that offer:
Intelligent automation to streamline administrative tasks and optimize workflows.
Personalization capabilities to create tailored patient experiences and foster trust.
Advanced technology solutions, such as behavioral AI, to automate patient interactions and improve care.
Here’s what market domination actually looks like.
The reality is that dominating a market requires that you’re doing things that others can’t match. If you have unlimited funds you can simply outspend the competition and suck up all the oxygen. (When I was running clinics my average spend per clinic was $40,000 per month.)
The better way is to build a much better patient experience, but you can’t do that with your current tools or by adding aromatherapy or whatever. You actually have to deliver value that no one else can match.
Fortunately, the newest healthcare technologies that have been developed for the enterprise and clinical trials that are now available.
The best of these is Storyline.
Clinics that have adopted Storyline have experienced a 4x increase in team productivity, a 260% increase in patient interactions without additional provider burden, and a 17% increase in total revenue [3]. And 96% of patients would recommend Storyline to their primary care physician, and give it 4.9 stars.
The landscape has changed, and clinics must adapt to compete effectively. By finding your unfair advantage - which is probably going to be tech - you can build a market dominating clinic.
References
Telemedicine's growth and potential:
"Telehealth: A Quarter-Trillion-Dollar Post-COVID-19 Reality?”
Description: This article discusses the rapid growth of telemedicine and its potential to become a significant part of healthcare services post-COVID-19.
URL: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality
The changing landscape of patient expectations:
"The Healthcare Consumer of the Future: How Patient Expectations Are Changing"Description: This article outlines the evolving expectations of healthcare consumers and the factors driving these changes.URL: https://www.forbes.com/sites/forbeshealth/2021/06/29/the-healthcare-consumer-of-the-future-how-patient-expectations-are-changing/?sh=1d4e40d07351
The importance of patient-centered care and relationships"The Importance of the Patient-Provider Relationship in the Digital Age"Description: This article highlights the significance of patient-provider relationships in delivering high-quality care and the role technology can play in strengthening these connections.
URL: https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0556
Clinician workload and the impact on patient care:
"Physician Burnout, Interrupted"
Description: This paper discusses the issue of physician burnout, its consequences on patient care, and potential solutions to address the problem.
URL: https://www.nejm.org/doi/full/10.1056/NEJMp2003149